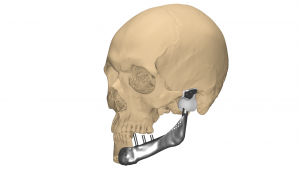
Custom TMJ Implant
Temporo-mandibular joint (TMJ) disorder causes pain, stiffness, or lack of mobility in the joint, keeping one from using the jaw’s full range of movement. An open joint surgery with replacement of complete TMJ by artificial prosthesis is required in severe TMJ disorder that involves complex tumors or trauma defects.
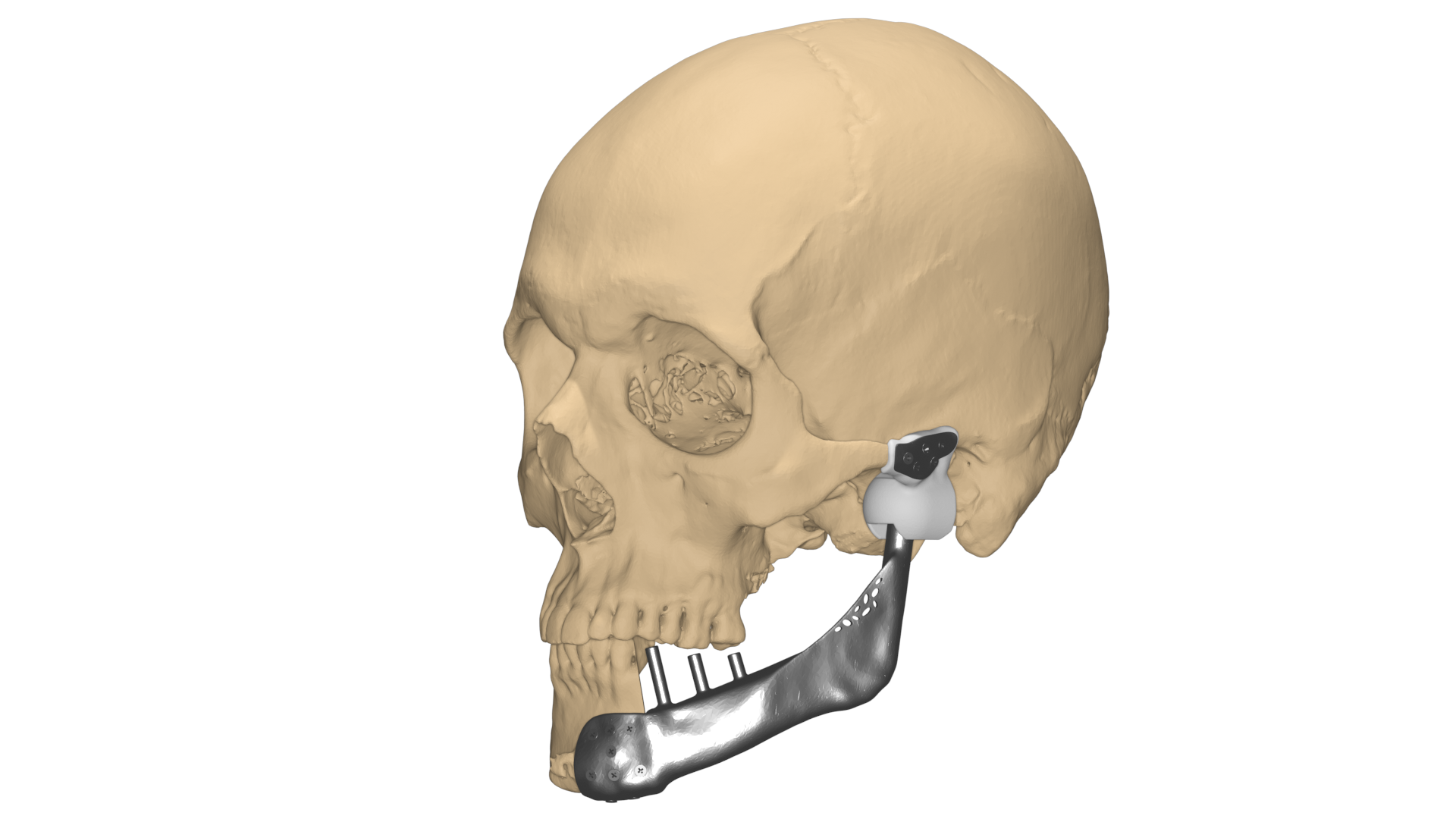
Here is one such case of TMJ replacement by using advanced visualization, pre-surgical planning, and customized TMJ implant for the patient. A male patient aged 26 had undergone a primary tumor removal surgery in the past and was required to reconstruct the deficient mandible with a customized implant.
Dr. Vivek Saxena, HOD, maxillofacial surgery unit –Army Hospital, approached our clinical engineers for a robust plan and precise reconstruction of the TMJ by using a patient-specific implant.
We mapped out to Visualize, Plan, and then execute.
Visualization:
To visualize the mandibular anatomy and its neighboring area, a high-resolution CT scan of adequate slice thickness and increment was used to 3D model the defect. The region of interest was well captured in the scan and replicated as a 1:1 digital model for understanding the defect and pathology. The idea is to provide a self-explanatory model and help the surgeon to make them visualize the information which usually remains hidden in conventional 2D CT images.

Planning:
Once the 3D modeling of the images (segmentation) was completed, the plan was to lay down the removal of the tumor followed by reconstruction using customized TMJ.
Key steps involved –
• Tumor on the left mandible was removed a year before including the condyle and hence, it was necessary to have the right occlusion and articulation when the TMJ is replaced.
• Healthy right mirror is mirrored to reconstruct the naturally curved mandible and the osteotomy cut is decided.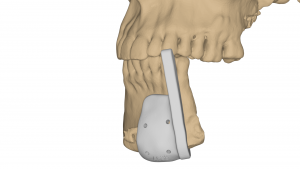
• Surgical guide was designed to resect the anterior mandible for perfect joint connection of implant body to the healthy right mandible
• To reduce the weight of the implant, there was a lattice structure provided inside the body, which also helps in osteointegration at the implant-bone contact surface.
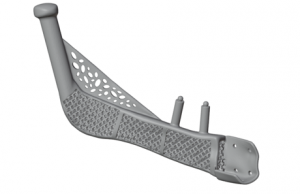
• To restore the teeth, the provisions – extruded dental abutment, were pre-defined in the mandible implant body accurately at the desired positions.
• Predefined holes – size, length, and insertion trajectory based on the bone density, on both body and fossa implant components.
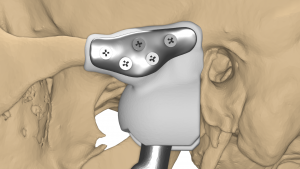
• Fossa was designed to ensure the proper range of motion of the implant and natural jaw opening, ensuring that the condyle does not dislocate out of the fossa.
• A virtual simulation was carried out to ensure appropriate jaw movements with the implant in place.
3D Printing:
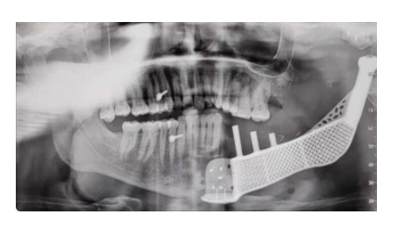
Once the surgical plan was approved and finalized, the plan was translated to physical models to analyze the outcome. Pre-op, intermediate, and post-op models were printed. The patient-specific guides were 3d printed in biocompatible autoclavable material for realizing the planned cuts intra-operatively on the mandible. The customized implant was printed in medical-grade titanium and the fossa was fabricated in high strength medical-grade plastic – UHMWPE with required finishing and post-processing techniques for better articulation.
Conclusion:
Preplanning the surgical approach and use of the customized surgical guides and patient-specific implant, helped in achieving accurate reconstruction, reduced intra-operative time, and faster recovery of the patient.
This case was recently talked about in TOI, here’s a small snippet

